Pan‑American Life Insurance Group
Trusted for over 110 years to take care of the important things in life, let us take care of you.
Insurance solutions help to protect your financial stability and safeguard your loved ones.


Pan‑American Life Insurance Group
Trusted for over 110 years to take care of the important things in life, let us take care of you.
Insurance solutions help to protect your financial stability and safeguard your loved ones.


Pan‑American Life Insurance Group
Trusted for over 100 years to take care of the important things in life, let us take care of you
Insurance solutions help to protect your financial stability and safeguard your loved ones.
Our Solutions
We will help you find the right solution to meet your insurance needs
For Individuals
Already Working With Us?
Find your portal
Our Solutions
We will help you find the right solution to meet your insurance needs
Already Working With Us?
Find your portal
For Individuals
For Individuals
For Employers & Sponsors
For Employers & Sponsors
For Agents & Brokers

23 RF
Financial Wellness Trends, Life Insurance
Do Stay‑at‑Home Parents Need Life Insurance?

Getty Images
Life Insurance
How Life Insurance Differs from Savings & Investment Products
FAQ
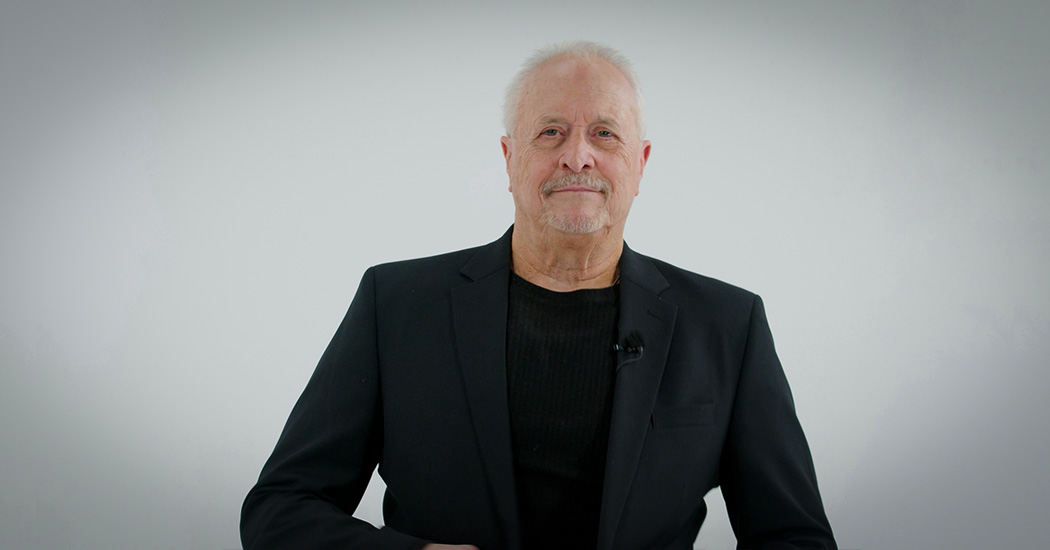
Testimonials
I was so impressed with the customer service you gave me. I’m sure that mine was not the biggest issue on your plate, but you treated me as if it was."
‑ Phil D. | Pan‑American Life Policyholder

Pan‑American Life has been responsive to all of my needs and the needs of my clients. It's created a bond; one that trust and support have everything to do with."